Welcome to WordPress! This is your first post. Edit or delete it to take the first step in your blogging journey.
Bridging Healthcare Gap
Connecting communities, saving lives.
recent posts
Take-Aways From Rubayat Khan’s TEDXDHAKA Talk
about
Author: Erros Dwayne Basilio Dineros, a BS Psychology student from Far Eastern University.
-
Bridging the Rural Healthcare Gap:
Take-Aways From Rubayat Khan’s TEDXDHAKA TalkHow do you ensure that people in rural areas who live miles away from the nearest clinic receive a real care and services? TEDXDhaka talk, “Bridging the rural healthcare gap,” challenged my presumptions about how “proper” healthcare looks outside the city.
The reality we don’t see

Dreamstime. (n.d.). Doctor and a patient in a rural village [Photograph]. Dreamstime. https://www.dreamstime.com/photos-images/doctor-and-a-patient-in-village.html Khan paints a stark picture from rural Bangladesh: Local pharmacy owner or “village doctor” is always the one providing healthcare service when people get sick. People don’t often see professionally trained doctors because official facilities are often miles away.
What struck me: While I often equated authenticity with credentials, I realized that access and trust are the first quality marks in rural areas. And dismissing this wouldn’t help patients who need care today.
Community lifeline from “quacks”
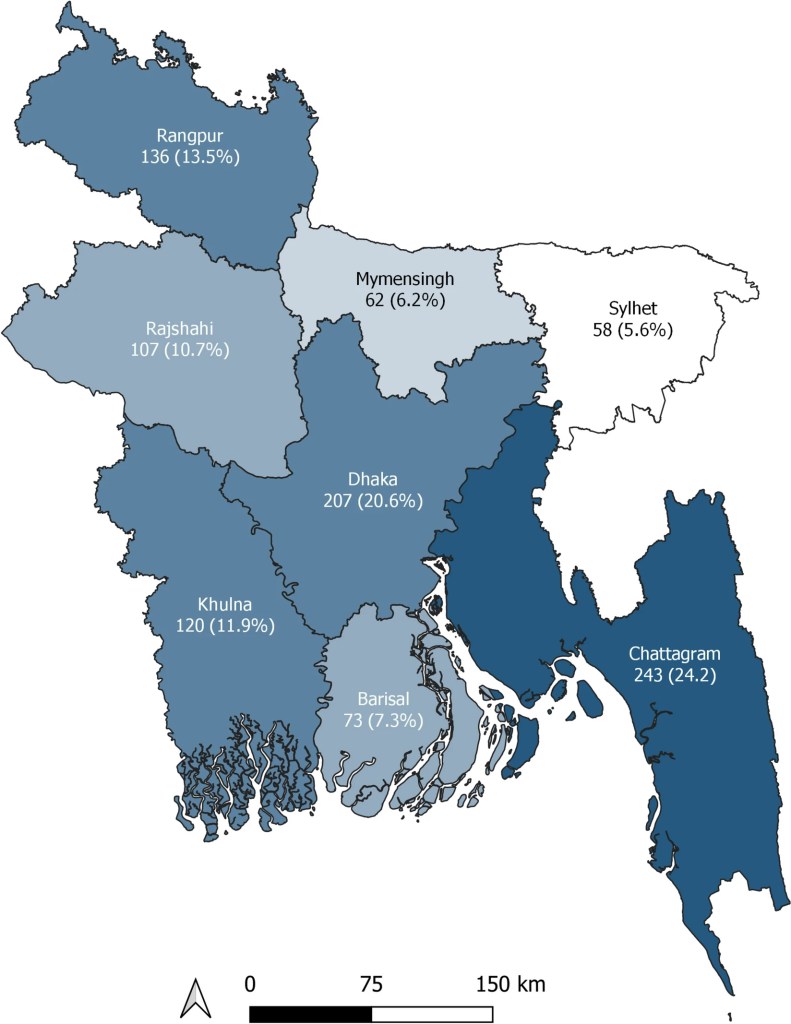
Alamy. (n.d.). Village doctor consulting patients in rural Bangladesh [Photograph]. Alamy. https://www.alamy.com/stock-photo/village-doctors-bangladesh.html Informal healthcare providers may lack formal training and overprescribe sometimes. But labeling them “quacks” can blind us to their value and to the possibilities of improving what they already do well. They are still embedded in the community, helping people willingly without appointments.
My take-away: I realized the fastest way to save lives to work with what exists and make it better; not to replace them with something perfect from scratch. Solutions often fail because they try to replace them entirely, instead of upgrading them.
Link, train, unite

The Borgen Project. (n.d.). Telemedicine in Bangladesh [Photograph]. The Borgen Project. https://borgenproject.org/telemedicine-in-bangladesh/ Khan’s proposed approach is strikingly practical:
- Telemedicine as a bridge: Improving the quality of primary services through technological advancements. Healthcare workers in rural areas can consult with urban physicians instantaneously.
- Specialized training: Equip informal providers with guidelines, triage competencies, and decision-making aids to reduce harmful practices and ensure consistent care
- Policy and market strategies: Incorporate these providers into the national system so that incentives are aligned with safer, evidence-based practices instead of banning their methods..
The essence of Khan’s organization, Jeeon, is to engage individuals in their own environments and leverage technology alongside market-driven motivation to connect with billions who lack dependable access to contemporary healthcare.
My take-aways from this:
- Perfection can be the opposite of what we need: Waiting for completely staffed rural hospitals will not help a patient who’s in need of antibiotics today.
- Policy equal reality: Accepting informal providers into the system—with training, supervision, and incentives—beats pretending they don’t exist.
- Trust is the foundation: Relationship with the providers is an asset, a foundation of trust and not a hurdle.
- Support throughout the journey: Distance, transportation, and expenses are also significant clinical concerns—telemedicine and triage procedures can be just as crucial as innovative medications.
Why this matters beyond Bangladesh

Getty Images. (n.d.). Health practitioners using telemedicine with rural patients [Photograph]. Getty Images. https://www.gettyimages.com/detail/photo/health-practitioners-using-telemedicine-with-royalty-free-image/1326646713 Although Khan’s speech is on behalf of Bangladesh, the core tension—scarce clinicians vs. abundant need is universal. Many rural regions face the same struggle: a very few specialists, long travel times, and reliance on community providers. The idea of link, trade, unite is well integrated because it’s built on human behavior and access, not just infrastructure.
A small action list I can start with:
- Learn the landscape: Who are the informal providers in a community and what do they already do well?
- Champion hybrid models: Support programs that train and digitally connect local providers to licensed clinicians.
- Ask better policy questions: Instead of “How do we eliminate informal care?” ask “How do we make it safer and more effective?”
Khan ends with a call to look for solutions in the grey areas—the messy spaces where real life happens. If we truly are serious about health equity, we’ll start strengthening the ones people already use and stop designing systems that only cater ideal conditions.